
The Impact of Multiple Intubations on Voice Change: A Case Study
The Impact of Multiple Intubations on Voice Change: A Case Study
Treatment for voice disorder
Reasearch
Method
A 78year old male with dysphonia from posterior glottic stenosis following prolonged intubations after coronary artery bypass graft, mitral valve replacement, and tricuspid valve repair was considered for the study. Written consent was collected from the client before the study.
The client reported voice change and difficulty in increasing the loudness. When the client continues to speak for a longer duration, he gets better voice quality for a short span of time (less than a minute) as reported.
Evaluation:
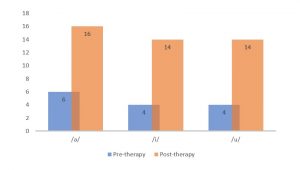
The voice assessment conducted included both qualitative and quantitative measures. Qualitative evaluation was performed using Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V) and GRBAS (Table 2) to assess the severity of the client’s hoarse voice, which presented with asthenia and absence of aphonia. The quantitative evaluation involved aerodynamic measurements, specifically Maximum Phonation Duration (MPD) and s/z ratio (Table 1). For both measures, the duration was measured using a stopwatch, and the phonation with the longest duration was selected from three trials.
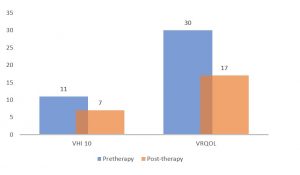
For the recording task, it was ensured that the client was seated in a noise free room and was asked to phonate /a/ at his comfortable pitch and loudness. The patient was asked to download the pitch tuner app and record the phonation sample. Self-perception of voice quality and its effect on quality of life was assessed through VRQOL and VHI 10 where the pre-therapy scores revealed a score of 30 (VRQOL) and 11 (VHI-10).
Table1: Aerodynamic measures of the client during assessment (before voice therapy).
| Pre-therapy | /a/ | /i/ | /u/ |
| MPD | 6 sec | 4 sec | 4 sec |
| S/Z Ratio | 1.5 | ||
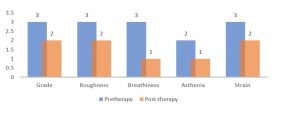
Table 2: GRBAS Results
| Pretherapy: | GRBAS |
| Grade | 3 |
| Roughness | 3 |
| Breathiness | 3 |
| Asthenia | 2 |
| Strain | 3 |
After the assessment, the client was advised to take voice therapy sessions. The sessions were carried out using the Zoom video conferencing platform from October to January.
Management
The therapy sessions included vocal hygiene education and semi-occluded voice therapy, breathing exercises, warm-up, stretching, and Auditory perceptual analysis for 1 session per week for 4 months. Self-assessment protocols were conducted before the intervention and 4 months after the last intervention, and the differences before and after interventions were compared.
Results:
The progress of the therapy was measured through a comparison of pre and post-therapy samples. Qualitative evaluation was performed using Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V) and GRBAS (Table 3) was performed at the end of 4 months revealing a moderate hoarse voice.
Table 3: Aerodynamic measures of the client during assessment (after voice therapy).
| Post-therapy | /a/ | /i/ | /u/ |
| MPD | 16 sec | 14 sec | 14 sec |
| S/Z Ratio | 1.3 | ||
Graph 1: Comparison of Pre and Post therapy MPD values
*Above values are in seconds
Table 4: GRBAS Results
| Post-therapy: | GRBAS |
| Grade | 2 |
| Roughness | 2 |
| Breathiness | 1 |
| Asthenia | 1 |
| Strain | 2 |
Graph 2: GRBAS Results Comparison
There was a significant reduction in VHI-10 and VRQOL scores by the end of 4 months
Table 5: VHI 10 & VRQOL comparison
| Post-therapy | Post-therapy | |
| VHI 10 | 11 | 7 |
| VRQOL | 30 | 17 |
Graph 3: VHI 10 & VRQOL comparison
The participant reported a lot of positive feedback from his family and colleagues with significant improvements in his overall quality of life.
Discussion and conclusion:
Millions worldwide suffer from voice disorders, affecting individuals of all ages. These conditions have a profound impact on quality of life, leading to social isolation, depression, and overall well-being decline. The study aimed to highlight teletherapy’s effectiveness as a voice therapy treatment. Results showed significant improvements in qualitative and quantitative measures, indicating progress in voice disorder treatment.
Tele therapists never run out of unique activities due to the benefit of technology. Right from Speech-Language Delays in children to Aphasia in adults we have got them all covered with our unlimited online resources. These findings can revolutionize voice therapy delivery and enhance the lives of those with voice disorders.
- The Impact of Multiple Intubations on Voice Change: A Case Study - August 18, 2023
- Is it Apraxia or Autism? - May 5, 2023

Leave a Comment
(0 Comments)