
Voice Therapy in the Context of the COVID-19 Pandemic: Guidelines for Clinical Practice
Voice Therapy in the Context of the COVID-19 Pandemic: Guidelines for Clinical Practice
Voice Therapy in the Context of the COVID-19 Pandemic: Guidelines for Clinical PracticeMoreThe As a result of the COVID-19 pandemic, health services have had to face a new scenario regarding patient care. The rapid advance of the virus and the large number of patients requiring medical care and hospitalization has become a major concern. Clinicians who work with voice disorders such as phoniatricians and speech-language pathologists (SLPs) must continue providing health services to patients in need. Let’s find out what researchers Castillo-Allendes and the team suggest for continuing voice therapy services in these times. Read the original article at click here
Challenges faced in Voice Therapy
In this context, voice therapy faces two challenges:
- intervention via tele-practice which is a feasible and useful alternative
- increased demand for services for risk of vocal impairment due to the COVID-19 disease itself
- secondary to invasive mechanical ventilation (IMV) in severe cases of the disease.
What was the purpose of the study?
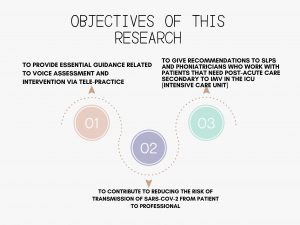
This study aimed to summarize some effective guidelines to promote safety and effective clinical practice. Specifically, this study had the following objectives:
Why was this study initiated?
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is transmitted through droplets. The clinicians who provide voice therapy, require an in-depth understanding of this disease to limit personal exposure and transmission of the virus. This risk increases during procedures such as voice evaluation and therapy. Regular speech, loud speaking, and singing generate air particles that could affect the probability of transmission of respiratory infectious diseases.
How was this study done?
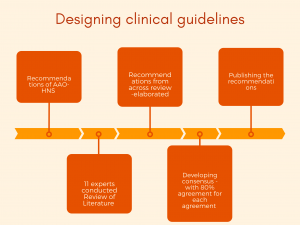
This manuscript was based on the recommendations of the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS). It specified clinical guidelines and was carried out by a group of experts in voice and swallowing disorders.
A total of 11 experts across the United States of America and Latin America were selected with three criteria. (1) to have more than 10 years of experience in the field, (2) to have a graduate education, and (3) to be currently working in a clinic, hospital, or academic institution.
Review for the formulation of guidelines consisted of clinical guidelines from various professional organizations/groups
Authors made the follwoing recommendations in this review..
Personal protection and prevention measures
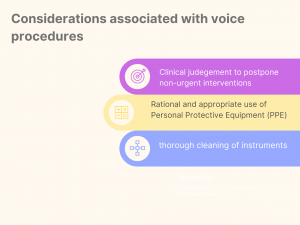
According to the World Health Organization (WHO), aerosol-generating procedures (AGPs) are defined as any clinical procedure that produces particles in the environment (aerosols), such as voice therapy, and instrumental voice evaluation. Hence to decrease the risk of infection, the following recommendations are made:
Considerations Associated with Voice Procedures
OSHA gave the classification of risk levels for occupational exposure to SARS-CoV-2. Voice clinicians may be at medium to very high risk.
Given below is a figure explaining Evaluation and Voice Therapy Procedures Organized According to Risk Levels for Occupational Exposure to COVID-19 Proposed by the OSHA
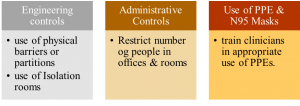
Recommendations for medium to high-risk situations, to improve occupational health safety:
The following suggestions for voice assessment are extrapolated from the CDC recommendations:
- Wear an N95 or higher level respirator, face shield, gloves, and a long sleeved-gown
- Limit no. Of people in the treatment room
- Carry out Voice evaluation in an airborne infection isolation room
- Maintain a distance of 1.8 m along with a sneeze guard or plexiglass
- Limit or avoid using headsets .
- Microphone placement should be 30cm from the patient’s mouth
- Visual/perceptual observations should be 1.8m
- Make appropriate judgments regarding laryngeal palpations
- Consider strategies that limit interactions to less than 15 mins
- Avoid using assessment tools which can’t be cleaned between patients
- Modify activity/task to reduce aerosolization
- Exercise hand hygiene
- For hospital-based SLPs: follow hospital guidelines
- Consider local reality
Considerations associated with the laryngeal endoscopic procedures
Laryngeal endoscopy, rigid or flexible requires a short physical distance between clinicians and patients and hence are highly risky. Moreover, sneezing and coughing is very common during the endoscopy procedure. Thus, making this procedure highly risky. Some guidelines for laryngeal endoscopies include:
- Apply local anesthesia in the nose by placing soaked pledgets
- Avoid sprays
- Schedule a COVID-19 test prior to the procedure
- Reschedule procedure if results are not available before the procedure
What are the new scenarios in Voice Assessment and Voice Therapy?
Tele-practice has emerged as an appropriate service-delivery model for speech therapists, more so, during the pandemic. However, it might not be appropriate in all circumstances. Decide the right candidates for tele-rehabilitation process with caution.
Some notes on Legal Framework and Ethical Challenges ….
Voice Therapy must almost always start with a laryngeal examination. This helps the clinician design the most effective treatment. However, laryngoscopy is an invasive procedure that put clinicians at risk, especially during this COVID-19 pandemic. A Speech-Language Pathologist can decide whether a patient will benefit from voice therapy even when laryngeal evaluation findings are not available. Determine the need for an immediate laryngeal medical evaluation.
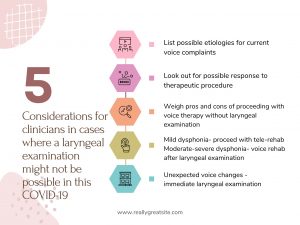
Some considerations for clinicians in cases where a laryngeal examination might not be possible in this COVID-19 pandemic situation:
Overview of Voice Assessment and Voice Therapy
What should a clinician consider for setting up a tele-practice?
- Clinicians should check the quality and speed of the session connection before starting.
- In addition, Use a quiet and well-illuminated space.
- Use an external microphone (adjustable and removable) to reduce ambient noise and optimize the auditory feedback.
- Make sure that the patient has good sound reception.
- Speak clearly, following vocal hygiene parameters.
- Use short sentences with easy-to-understand information.
- Maintain a proper posture in front of the computer
- Use the chat feature to reinforce information when the internet connection is not stable
What are the recommendations regarding Early Approach after Invasive Mechanical Ventilation or in ICU settings?
- Perform risk-benefit analysis for intervention
- Prioritize cases with severe laryngeal damage
- Reduce the time of visits
- Dispose Tubes, straws, respiratory devices after one-time-use
- Use short questionnaires or specific questions in the assessment
- Use Maximum Phonation Time (MPT) to understand closure defects and swallowing disorders
- Evaluate general respiratory coordination to assess airway protection during swallowing
- Employ Semi-Occluded Vocal Tract Exercises and Resonant Voice Exercises
- Use caution while using exercises with water
- Practice voice exercises as a complement to swallowing exercises
- For Post-intubation phonatory insufficiency, use exercises favoring glottal closure, improve swallowing and phonatory functions
- More important, avoid exercises that trigger cough or droplets such as trilling
- Provide vocal hygiene habits
Recommendations for psychosocial considerations linked to voice therapy and teamwork
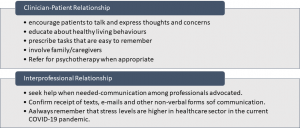
Stressors associated with the COVID-19 pandemic can negatively affect voice quality. The following recommendations are suggested for
Read more about Voice Care tips
In conclusion ….
The authors included recommendations related to the use of PPE, techniques to reduce the risk of spreading the virus. They also recommend performing voice assessment and treatment in the hospital setting and through tele-practice.
The authors, in this review, immediate guidance for voice therapists treating patients during the COVID-19 pandemic.
- “Interventions for children and adolescents with stuttering” - April 7, 2023
- What is Speech Therapy and its effect? - December 21, 2022
- Dysphagic disorder in a cohort of COVID-19 patients - December 13, 2022




Leave a Comment
(0 Comments)